Like other healthcare purchasers, the 32BJ Health Fund is not immune to the forces causing healthcare prices to rise. What’s different is the way the Health Fund responds. Many payers choose to raise premiums, copays, deductibles, and other out-of-pocket expenses—and shift more of the financial responsibility from employers to employees. The Health Fund does everything possible to avoid taking such action because we know that high prices can be a barrier to treatment for our participants.
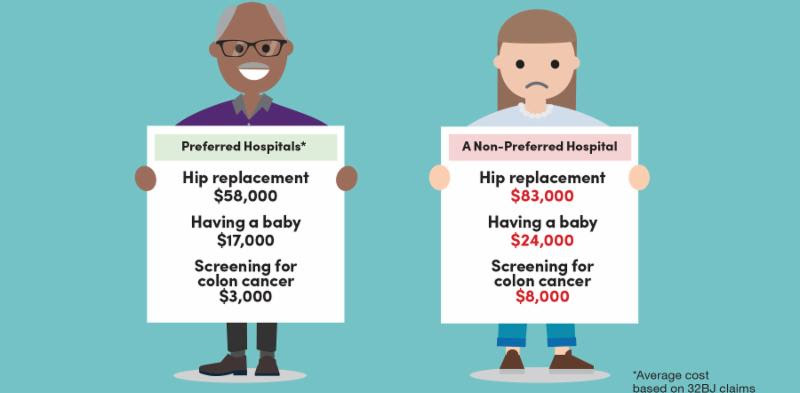
To control our expenditures, we developed a robust data analytics team to analyze the millions of rows of claims data we receive from our partners and vendors. The findings revealed major variations in the prices we pay for standard, high-volume procedures at New York City hospitals. For example, the Health Fund paid more than $80,000 for hip replacement surgery at one hospital, as opposed to a median price of $53,000 elsewhere. There were similar price disparities for having a baby, knee replacements, and many other kinds of inpatient and outpatient care, but there was no evidence of quality differences to support the higher prices.
Communicating clearly and authentically to educate participants and preserve their trust
While most Health Fund participants were already using preferred hospitals, our goal was to encourage even more of them to use preferred hospitals when they needed hospital-based care. We developed a communications campaign to inform plan participants of what we were changing—and why—and to help them find preferred hospitals for care and ensure they would know how to get help if they needed it. Ultimately, we wanted to maintain the favorable view most participants had of their health plan and their trust in the Health Fund.
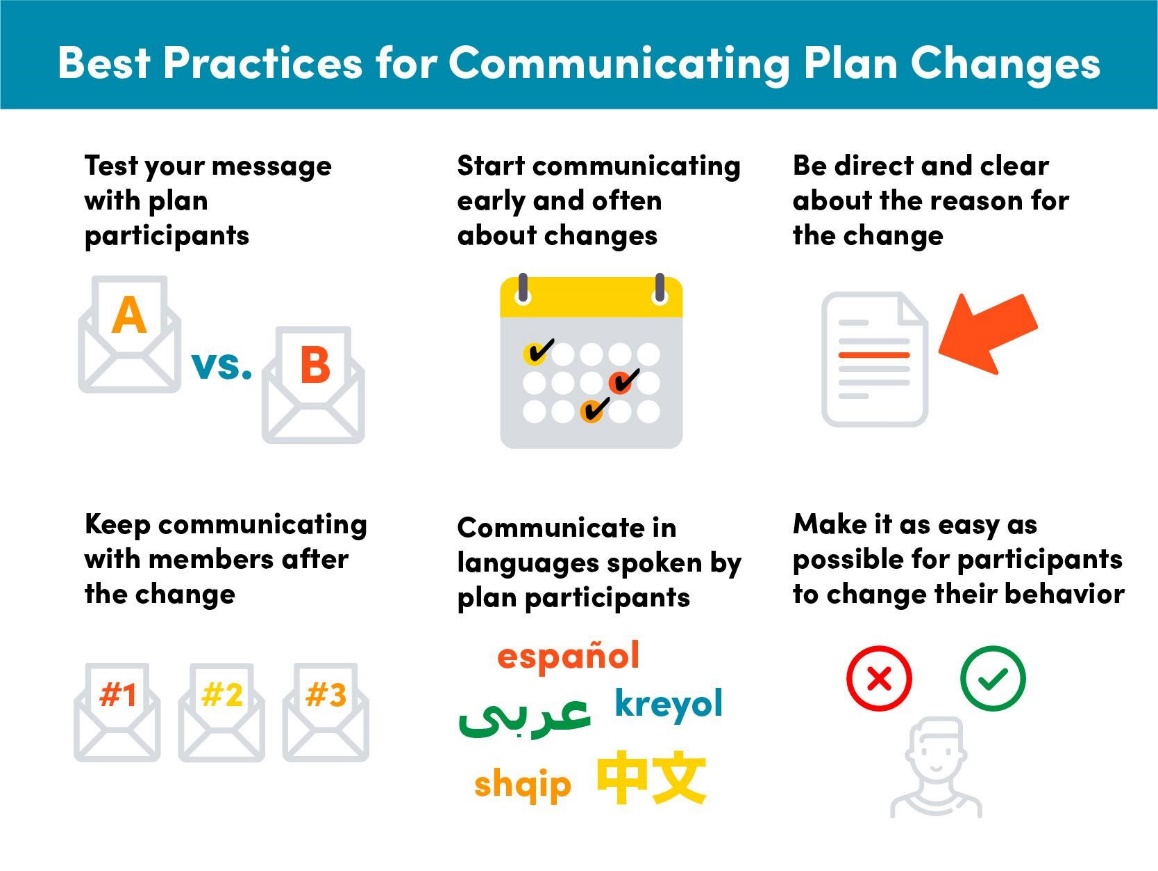
We already knew that our participants preferred receiving benefit information at home, so our plan was to communicate early and often through a variety of formats and languages, including two to three mailers each month in the three months leading up to the change. The Health Fund created additional mailers with messaging tailored to participants who had used nonpreferred hospitals and to participants in our maternity program, who would give birth in the coming months. To utilize all trusted communications channels, we also partnered with the union to educate members at their worksites and at union meetings, and we developed a series of emails that linked to information on our website in the weeks leading up to the change. We produced all communications in English and Spanish, the two languages spoken by the majority of plan participants. The mail program included a mix of federally mandated letters and a series of accessible and engaging pieces that were easy to read and clearly outlined the network change in simple language. The centerpiece of the campaign was a glossy, eight-page brochure that presented the most compelling arguments and offered a pull-out card with specific questions that participants could take to their doctor if they had upcoming inpatient or outpatient care, so that they could make sure they’d be treated at a preferred hospital with a low copay.
Once we implemented the network change, we evolved our educational campaign to reinforce the advantages of preferred hospitals. We also monitored our claims data and sent a letter to each participant who received care at a nonpreferred hospital, explaining the new network design and their options to receive care with lower copays—a practice we continue to this day.
 Getting the message right
Getting the message right
To optimize our strategy, we conducted focus groups of participants, including spouses, who are often partners in a family’s healthcare decisions, and polled more participants to hone our messages. Our research confirmed that messages that detailed the network change and outlined the rationale for our decision resonated most strongly.
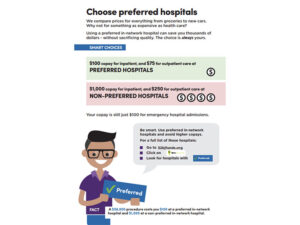
The top testing message said that the Health Fund had provided generous benefits with a $100 hospital admission copay for the last five years, but skyrocketing New York City hospital prices were making it untenable to maintain our current copay structure. Further, the message gave examples of the wide variation in prices that hospitals charged to perform the same procedures and explained that the Health Fund was implementing the new copay structure and encouraging participants to go to preferred hospitals for care so that we could keep their copay at $100.
Four months after the change, the Health Fund commissioned a poll of 600 participants who had used hospital services in the previous 12 months to gauge their reaction to the network change. We learned that while participants’ general understanding was good, we would need to do more to improve their familiarity with and perception of the change.
Equally important, the results confirmed that the Health Fund remained in great standing with our participants, the majority of whom reported that they viewed their benefits, the quality of in-network facilities and doctors, and the number of facilities and doctors near them “very favorably.” Nearly 9 in 10 plan participants said they trusted the Health Fund to recommend benefit programs; nevertheless, users of nonpreferred health systems were less likely to have the same level of trust.
Our research also revealed communication opportunities. For example, only a third of participants said they were familiar with any change for hospital admissions, and fewer than a third said they were “very familiar” with the copay change. When we explained how and why we changed the copay structure for inpatient and outpatient admissions, the majority said that while they understood that the Health Fund pays some hospitals more for the same services, they “strongly opposed” the change to the copay structure. This response would seem to suggest that the communications resonated with participants, and even if our messaging did not ameliorate their view of the change, participants did not hold the decision against the Health Fund. Perhaps the most important insight the data revealed is that in the six months following the plan change, an increasing number of participants had moved to preferred hospitals for planned hospital visits.
© 2019 32BJ Health Fund; Revised 2023